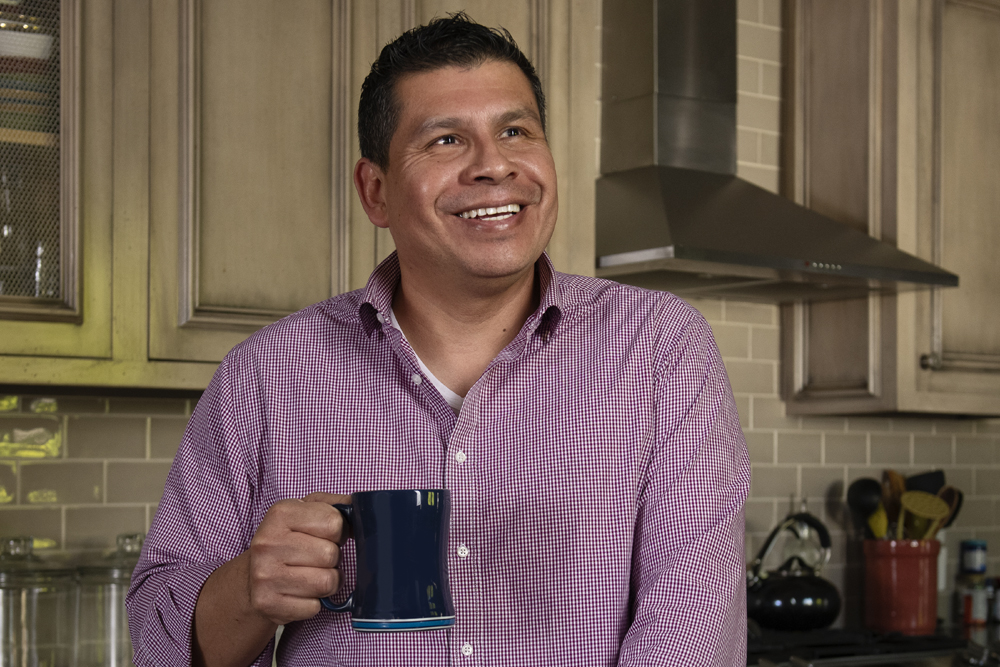
Jose Salas had been dealing with sleep apnea for 15 years. Instead of joining colleagues for lunch at work, he often napped in his car in a vain attempt to catch up on sleep.
So, when Salas walked into the USC Sleep Apnea and Snoring Surgery Center in 2017, he was beyond exhausted.
Salas’ memory took a hit, too. He soon found himself struggling to remember where he put things or what time he needed to be somewhere.
The absolute worst part of chronic sleep deprivation, he says, was knowing that he was sometimes short-tempered with family, friends, and work colleagues even though they were never the source of his sour moods. Sleep deprivation had robbed him of his cheerful nature and innate positivity.
“I was just so tired all the time, and I didn’t feel like myself,” says Salas, 45, who first experienced excessive sleepiness around the time he turned 30. He was young and trim, had no other medical problems and was not a smoker or heavy drinker.
In other words, he wasn’t an obvious candidate for sleep apnea. But, after checking in to a sleep clinic, he learned that was the cause of his problem.
Struggling to breathe at night because of sleep apnea
An estimated 22 million Americans have sleep apnea, mostly obstructive sleep apnea (OSA), in which blockage of the airway in the throat interrupts breathing throughout the night.
Normally, people go through various stages of sleep, the deepest of which is rapid eye movement, or REM, sleep. OSA disrupts these cycles and can prevent a person from entering the deepest stages of sleep.
This inability to experience sustained rest results in excessive tiredness and other symptoms during the day. Research into OSA in recent decades has shown that it may be far more detrimental than just causing problems with alertness during the day.
Sleep apnea linked to other serious health issues
Increasingly, sleep apnea has been associated with high blood pressure, diabetes, cardiovascular problems, depression, anxiety and numerous other serious medical conditions.
In other words, sleep apnea is no longer swept aside as a condition that only affects a person’s quality of life. It is understood now that improving sleep can help people live healthier lives. And yet, for some patients, including Salas, finding an effective treatment can be a struggle.
By the time he met Keck Medicine of USC’s Eric Kezirian, MD, MPH, one of the few surgeons in the country who specializes in sleep apnea and snoring, he had tried numerous methods including three separate surgical procedures.
“He was getting poor sleep every night,” says Dr. Kezirian, professor of sleep medicine and surgery in the USC Caruso Department of Otolaryngology – Head and Neck Surgery at the Keck School of Medicine of USC.
“We all are tired, have changes in our mood or experience fatigue and difficulty concentrating when we do not get a good night of sleep,” Dr. Kezirian says. “The problem with Mr. Salas was that he never was able to have a good night of sleep, so he was feeling this all the time.”
A family member had read that Dr. Kezirian was using a new device that encourages upper airway stimulation. Salas was hoping he would be a candidate for the device because he had tried just about everything else and nothing helped.
At-home sleep apnea remedies are not always effective
After his first sleep study 15 years ago, Salas hoped that getting a diagnosis would mean relief and that a good night’s sleep was within reach.
He tried a continuous positive airway pressure device, known as a CPAP machine, which blows a stream of air into the airway through a mask. The device keeps the airway open during sleep.
He knew the machine helped others, but it did not work for him. The machine often fell off when he turned over in bed. It took his wife some time to acclimate to the sound of his breathing while using CPAP.
The machine made a distinctive sound, to say the least. “My kids are the ones that figured it out,” Salas remembers. “My youngest is three, and he said, ‘Oh Daddy, you’ve got the Darth Vader mask on.’ And I said, “Yeah, I do. I have it on.”
He also developed chronic sinus infections while using the device despite cleaning his machine meticulously. Salas also used other treatments, such as a neti pot and over-the-counter drugs, to keep his sinuses clear. He tried a custom mouthguard, which he liked, but it did not help him sleep.
Personal approach to sleep apnea treatment
One doctor repaired Salas’ septum, hoping that would help. Another thought scarring from the first surgery impaired his breathing and operated on him a second time to fix that.
A third removed his uvula, the structure that extends down from the soft palate in the back of the throat. These helped a little, but he was back on the CPAP machine, and struggling with it, shortly afterward.
Most surgeons are trained with a single surgical procedure for all patients. But research has shown that this one-size-fits-all approach is not successful for most patients.
One of Dr. Kezirian’s areas of expertise is using state-of-the-art approaches to evaluate each patient to determine what surgery will work best for them.
Endoscopic evaluations allow customized surgical plans
Dr. Kezirian is an expert in the use of drug-induced sleep endoscopy. It’s an evaluation that involves threading a camera through the nostril while the patient is sedated in the operating room.
This allows Dr. Kezirian to see exactly which structures in the throat are causing a breathing blockage, allowing him to create a personalized surgical plan for each patient.
“I wake up in the morning and instead of being tired, I am good to go.”
Jose Salas, patient, USC Sleep Apnea and Snoring Surgery Center
“There are different procedures available for sleep apnea, but you want to tailor it to each person,” says Dr. Kezirian, “and that is what the evaluation procedure does.”
Dr. Kezirian evaluated Salas using this method and learned he wasn’t a candidate for upper airway stimulation due to the type of blockage he had.
Innovative surgical techniques to treat sleep apnea
Instead, Dr. Kezirian said he could help him using a newer surgical technique called expansion sphincter pharyngoplasty which involves removing the tonsils and repositioning the tissues of the soft palate and sides of the throat.
“I was a little hesitant to have another surgery until he explained the evaluation and what he found,” says Salas, who had never been evaluated using drug-induced sleep endoscopy by other doctors.
“Dr. Kezirian was able to show me where I was getting the obstruction. That was the first time I had seen anything like that.”
After the evaluation, Salas decided to embrace the old adage about the third — well, fourth — time being the charm and agreed to Dr. Kezirian’s surgical plan.
Several months later, Salas is doing things at home and work that he could not have imagined a few years ago. He has taken on new responsibilities at work and is enjoying new challenges for the first time in years.
Instead of going home and collapsing on the sofa, he often takes his kids to the park to kick around a ball. His most recent sleep study showed that his sleep apnea is no longer interfering with breathing at night.
But Salas says he didn’t need that study to know that Dr. Kezirian’s surgery had worked.
“I wake up in the morning and instead of being tired, I am good to go,” Salas says.
Topics